The bacterium Helicobacter pylori is dangerous because in most infected people it gives no symptoms, but almost always causes changes in the gastrointestinal tract, at least gastritis.
Many people are frightened that in order to detect Helicobacter pylori and prescribe a suitable treatment, it is necessary to undergo fibrogastroduodenoscopy (swallow a probe, as they say popularly), during which pieces of tissue are taken. In fact, this is not always necessary. There are breath tests for helicobacter, PCR analysis of feces.
In what cases can non-invasive methods of investigation be used and how do doctors now select effective drugs against Helicobacter pylori? Elena Fyodorovna Kachanko, Head of the Infection and Epidemiology Department of the State Institution “Republican Clinical Medical Center”, told about the most modern approaches.
— Elena Fedorovna, how many people are infected with Helicobacter pylori? How is this bacterium transmitted?
— Helicobacteriosis is the most common chronic infectious disease today. The Helicobacter pylori microorganism that causes it is all around us, so the infection spreads easily.
The main way of infection with Helicobacter pylori is through household contact. This means that you can “catch” the infection through common household items on which the saliva of the carrier of this microorganism remains (through furnishings, household appliances, toys, dishes, cutlery, door handles, hygiene items). For example, drinking from someone else's mug or from poorly washed dishes in places of public catering. There is a very high probability of Helicobacter pylori transmission in the family, as well as in children's groups - kindergartens, schools, camps.
You can get infected with Helicobacter pylori and fecal-oral route, if you do not observe personal hygiene rules (do not wash your hands after the toilet, before eating). In this case, the infectious agent is localized mainly in the gastrointestinal tract of a person, is excreted from the body with feces or vomit.
Penetration into a susceptible organism occurs through the mouth, after which it re-localizes in the digestive tract of the new organism. Infection occurs through unwashed vegetables, fruits, hands, unfiltered, raw water. This also includes expired foods and foods that have not been sufficiently heat-treated.
Our Russian colleagues conducted a study that showed that 70-80% of people in Russia are infected with Helicobacter.
Foreign researchers have concluded that the better sanitary-epidemic and hygienic actions are carried out in the country, the less infection with this microbe. That is, if you and I wash our hands always when we need to, we will protect ourselves from meeting this microorganism.In addition, the Russian researchers shared the observation that not only did the number of intestinal infections decrease, but Helicobacter infections dropped from 80 to 50 percent during the covid, when people were more diligent about hygiene.
— What diseases does Helicobacter pylori cause?
— Helicobacter pylori most often (in 80% of people) causes gastritis. It can also cause gastric ulcer, duodenal ulcer, MALT lymphoma. And, of course, the worst disease caused by Helicobacter in every sense is gastric adenocarcinoma, i.e. stomach cancer. It occurs only in 3-4% of cases, but it does occur, so it is important to diagnose and treat this infectious disease in time.
— How quickly do the effects develop after infection?
— Everything is very individual and depends on many factors. If Helicobacter has settled in a pale girl with low iron, anemia, heavy menstruation, it is certain that she will develop disorders faster than a healthy person with normal hemoglobin.
Also more susceptible to Helicobacter, such as people with cirrhosis, low platelets.
— Who should get tested for H.pylori?
— The major diseases caused by H.pylori traditionally include peptic ulcer disease, MALT lymphoma, gastric adenocarcinoma and dyspepsia.
Additional associations with idiopathic thrombocytopenic purpura unexplained iron deficiency have been established.
New evidence suggests that patients taking long-term nonsteroidal anti-inflammatory drugs, including low-dose acetylsalicylic acid, are more susceptible to infection.
Testing is recommended for people at increased risk of developing gastric adenocarcinoma (e.g., patients with autoimmune gastritis, precancerous conditions, or first-degree relatives with gastric cancer) and those who live with people who test positive nonserologically for H.pylori.
— How is Helicobacter detected? In which cases are invasive methods used and in which cases are non-invasive methods used?
— Gastritis, an inflammatory process in the gastric mucosa, is not a clinical diagnosis, but a morphologic one. That is, gastritis is not established on the basis of symptoms, but only on the basis of fibrogastroduodenoscopy (FGDS), during which several biopsy specimens from different parts of the stomach are necessarily taken.
But the complaints that a person presents (heartburn, nausea, vomiting, pain in the epigastrium - the upper part of the abdomen) are called dyspepsia.
Regardless of whether a person has any clinical manifestations of gastritis, if Helicobacter pylori bacterium is found, it is necessary to undergo a course of antibiotic therapy.So, if an FGDS is performed, biopsy specimens (pieces of tissue) are definitely taken for examination - and the microbe is either detected or not detected.
However, there is a group of young patients (up to 45-50 years old) without complaints that would make them do a gastroscopy, but with a desire to be tested for Helicobacter. Non-invasive tests are performed for them.
The urease breath test is widespread in Belarus. Urease is an enzyme that is secreted by Helicobacter pylori. Therefore, if the microbe is present in the patient's body, the respiratory urease test will show it.
However, even if a person is young, without noticeable problems with the gastrointestinal tract, but his mother, father, grandmother, grandfather had stomach cancer, this method of investigation is not suitable for him. We need to do a gastroscopy.
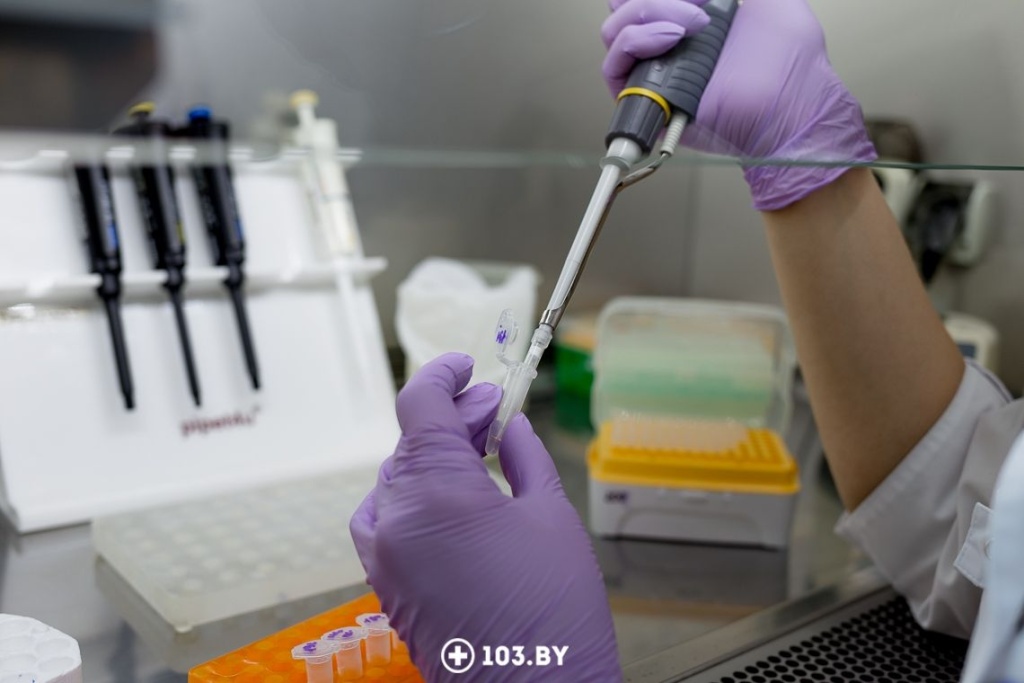
The newest non-invasive method of testing for Helicobacter is PCR stool analysis.
- PCR test is recommended for people with symptoms of gastrointestinal problems - if there are complaints of stomach pain, heartburn, nausea or frequent digestive disorders.
- People with ineffective treatment for ulcers or gastritis should also undergo a PCR test for Helicobacter. If symptoms do not go away even after taking antibiotics, the cause may be antibiotic resistance of the bacterium.
— What are the advantages of a PCR test?
— PCR diagnostics is characterized by high accuracy and sensitivity. It helps:
- accurately confirm the presence of infection - we can find the genetic material of the microbe, even if the amount is negligible;
- determine bacterial resistance to macrolides;
- avoid unnecessary antibiotics;
- create an individualized treatment plan that will increase the chances of successfully getting rid of the infection.
Thanks to modern diagnostic technologies, treatment for Helicobacter pylori is maximized. Instead of the standard “trial and error” approach, doctors can use a personalized approach, taking into account the specifics of the infection in each patient.

— How is treatment against Helicobacter pylori selected?
— In the past, the gold standard for diagnosing Helicobacter pylori was the bacteriologic method of testing. It requires taking a piece of tissue, sowing it on a Petri dish, waiting for the microbe to grow, obtaining a pure culture of the microbe and then only determining sensitivity or resistance to antibacterial drugs.
Now it is done more easily. The newest and already available in the Republic of Belarus method is polymerase chain reaction (PCR). This is a molecular-genetic method with the help of which it is possible both to find the microbe and to examine it for resistance to certain antibacterial drugs.
Experts who deal with Helicobacter now recommend mandatory testing for Helicobacter pylori resistance, especially to macrolides (particularly clarithromycin), the drugs that are part of the first-line therapy against Helicobacter.
The fact is that, as European and American colleagues write, they have very high resistance to clarithromycin - at the level of 30%. That is, out of 100 people who will be treated with clarithromycin, 30 patients will not respond.
Russian colleagues also conducted such a study. They write that their resistance rate does not reach 15%. It is believed that at this rate, macrolides can still be used as first-line therapy. If resistance is higher than 15%, a different regimen should be used.
Today there are 4 regimens of therapy. The first one is necessarily clarithromycin, amoxicillin and some proton pump inhibitor (most often omeprazole). For 14 days the patient takes antibiotics. Testing for cure of H.pylori should be done at least after 4 weeks. Testing is performed by urease breath test, fecal antigen test, or gastric biopsy.
We, at the Republican Clinical Medical Center, have available tests to determine resistance to clarithromycin. We perform PCR analysis, which, I remind you, can detect Helicobacter pylori not only in gastric biopsy but also in feces. This is especially important when it is necessary to check whether the therapy has been successful, because every time a gastroscopy is not the most pleasant option for the patient.The PCR test is fast and results can be obtained on the day of submission.

— How does a two-week course of antibiotics affect the body? Seems like a pretty aggressive therapy.
— Of course, antibiotics are not vitamins. All antibacterial drugs have side effects, because the gastric microbiome is disturbed. Especially, indeed, the course for Helicobacter is always 14 days, whether it is first, second, third or fourth line therapy.
The worst thing about antibiotic use is the rise of antibiotic resistance. By taking them frequently and in large quantities on and off occasion, we reduce the possibilities of antibiotic therapy. So it's better to prevent bacterial diseases. And this is, as I said, banal hygiene.

Interviewer: Christina Goloviychuk
Photo: Anna Zankovich
103.by